
UMN Medical School researchers from the Masopust lab have offered new ways to think about the immune system thanks to a recent study published in Nature. Their research, led by Sathi Wijeyesinghe, Ph.D., indicates organ tissues become increasingly immune throughout life, these findings may begin to alter fundamental ideas regarding the rules of vaccination and the immune system's function within the body.
New findings suggest organ tissues become increasingly immune throughout life
Author: | April 20, 2021
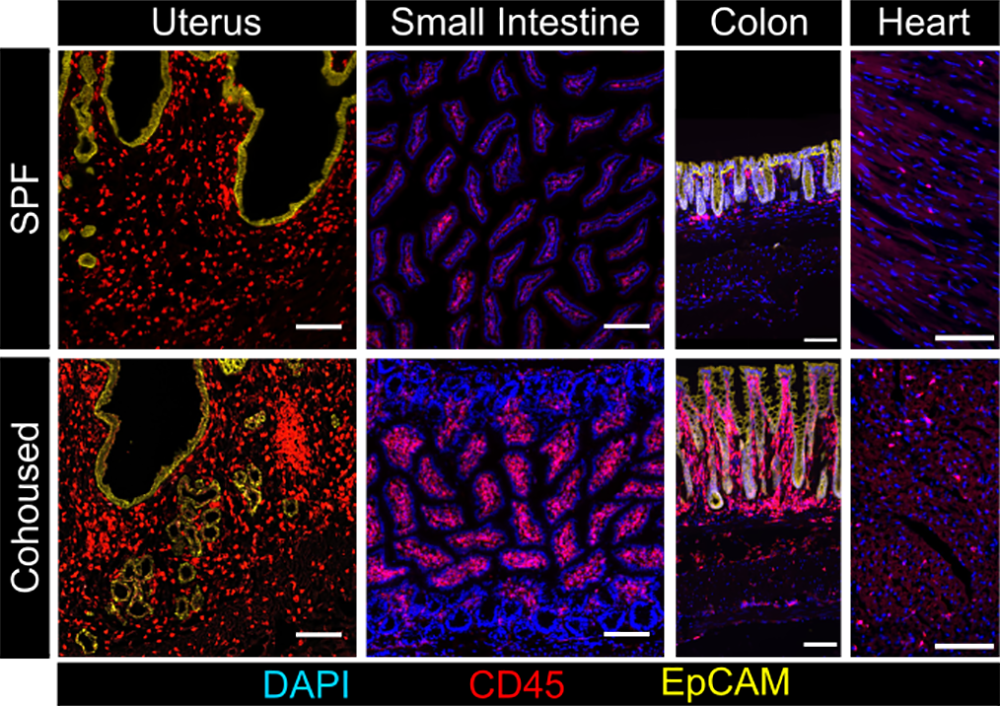
Photo: Cohousing specific-pathogen-free mice with pet shop mice reveals an expansion of tissue immunities in response to human-like microbial experience
MINNEAPOLIS/ST.PAUL (04/20/2021) — University of Minnesota Medical School researchers have offered new ways to think about the immune system thanks to a recent study published in Nature. Their research, which indicates organ tissues become increasingly immune throughout life, may begin to alter fundamental ideas regarding the rules of vaccination and the immune system’s function within the body.
Sathi Wijeyesinghe, PhD, the lead author on the study is a researcher in the Masopust Lab at the U of M Medical School, which focuses on T cell immunity. His research began with the goal to understand the lifespan of T cells in organ tissues, which are known to fight off viruses while also protecting from reinfection by the same virus.
“Historically, studies of the immune system have emphasized its renewable nature through bone marrow, lymphoid organs and blood. Our work shows how much this model fails to account for the many immune cells distributed throughout other organs of the body, where most infections and tumors arise,” Wijeyesinghe said. “What we found ends up painting a much broader picture of how the immune system accomplishes surveillance of the entire body for pathogens, tissue damage and tumors.”
The study’s major findings, include:
- Antiviral T cells that reside in most organs of the body persist over time and in the face of extensive infectious exposures;
- Unlike other organ systems, the immune system becomes increasingly immune throughout life, which is a natural response to accumulated microbial exposures over time;
- Up to 25% of the cells in organs were immune cells, indicating that the immune system significantly contributes to the cellular makeup of the body;
- And, along with antiviral T cells, most other immune cells are durably tissue-resident in organs as well.
Wijeyesinghe hopes this study can further advance the ongoing change in how the broader scientific community conceptualizes the immune system and immune homeostasis.
During this study, Wijeyesinghe also unexpectedly discovered how tissue-resident T cells may serve as the origin for memory T cells in blood. As a next step in this research, the Masopust Lab is developing new techniques to trace the fate of these immune cells, hoping to further dissect the relationship between blood-borne and tissue-based immunity.
This study is funded by University of Minnesota Medical School, the National Institutes of Health grants (R01 AI084913, R01 AI146032, F30 DK114942 and T32 AI007313) and Howard Hughes Medical Institute Faculty Scholars program.